
September 2025 | By Softheon
Key takeaways for payviders:
- Affordability thresholds are shifting. Enhanced subsidies are set to expire, creating uncertainty around 2026 premiums and APTC levels.
- Member communication will be critical. Renewal notices won’t include full premium or subsidy details, so payviders must lean on brokers, digital channels, and proactive outreach to reduce confusion.
- ICHRA and diversification are on the rise. With group markets shrinking, more employers are exploring ICHRA, opening new opportunities for payviders that can flex their infrastructure.
Open Enrollment 2026 (OE26) is shaping up to be one of the most complex enrollment seasons in recent memory. With subsidy uncertainty, rising premiums, and shifts in the group market, payviders face both new challenges and emerging opportunities.
In Softheon’s first LinkedIn Live, leaders came together to explore how affordability threshold changes will affect members, brokers, and health plans — and what payviders can do to prepare.
A New Kind of Enrollment Season
One of the biggest variables heading into OE26 is the status of enhanced subsidies first introduced in 2021. Unless Congress acts, these supports will expire at the end of the year, dramatically raising net premiums for many families. Middle-income households could face sharp increases, reshaping affordability across the Marketplace.
At the same time, new eligibility and enrollment rules are shifting the process itself. Manual income verification, changes in re-enrollment policies, and evolving notice requirements all create a more complex environment for members who have grown used to automatic renewals.
As Marc Bryant, SVP of Healthcare Solutions, explained, “We’re preparing for a season of higher premiums, potentially higher member churn, and higher service demand. Plans should expect call centers and retention teams to feel the pressure.”
Charles Gaba at ACASignups.net released his preliminary weighted 2026 rate filings for all 50 states and the District of Columbia. As of early September, ACA premiums for OE26 will increase on average by 23.4%.
Group Coverage Under Pressure: The ICHRA Opportunity
The affordability threshold change isn’t just an Individual market story. Small and mid-size businesses are struggling with the rising cost of traditional group coverage, and more are exploring alternatives like the Individual Health Reimbursement Arrangement (ICHRA).
Josh Schultz, Head of Government Affairs, pointed out that “the group market continues to shrink. Small and mid-size employers are dropping out, and we’re going to see more and more initiatives through ICHRA and QSEHRA to find alternatives to traditional group coverage.”
ICHRA allows employers to fund tax-advantaged stipends that employees can use to purchase their own individual health insurance. For payviders, this trend has two major implications:
- New revenue streams: Employer-funded stipends are fueling enrollment growth in the individual market, expanding the pool of members that community-based health plans can serve.
- New operational demands: Unlike group coverage, ICHRA introduces greater complexity — with multiple Third-Party Administrators (TPAs), benefit platforms, and Marketplaces all handling eligibility, enrollment, and payments in different ways.
Marc explained during the session, “ICHRA is opening up a pipeline of employer-funded members, but they also bring tighter data requirements and higher churn in thin-margin markets. Payviders need to be ready with the right balance of enrollment, pricing, and service infrastructure.”
This shift isn’t hypothetical. Adoption is climbing quickly, with nearly half of large employers considering ICHRA as an option for their workforce. For payviders, that means an opportunity to capture new membership if their infrastructure can flex to meet employer and employee needs.
Brokers on the Front Line of Retention
Brokers remain the front line of member support during renewal season. Rising premiums, subsidy shifts, and notice changes all converge at the point of member decision-making — and brokers are the ones navigating that complexity with clients.
For payviders, enabling brokers with the right tools can make the difference between retention and attrition. Rate sheets, comparison guides, and scripted FAQs allow brokers to respond quickly and confidently to member concerns.
Lindsey Miller, Program Director of Health Plan Solutions, emphasized the point, “Brokers are the most powerful retention channel. If they’re confident, members will be confident — and that’s how you keep enrollment steady.”
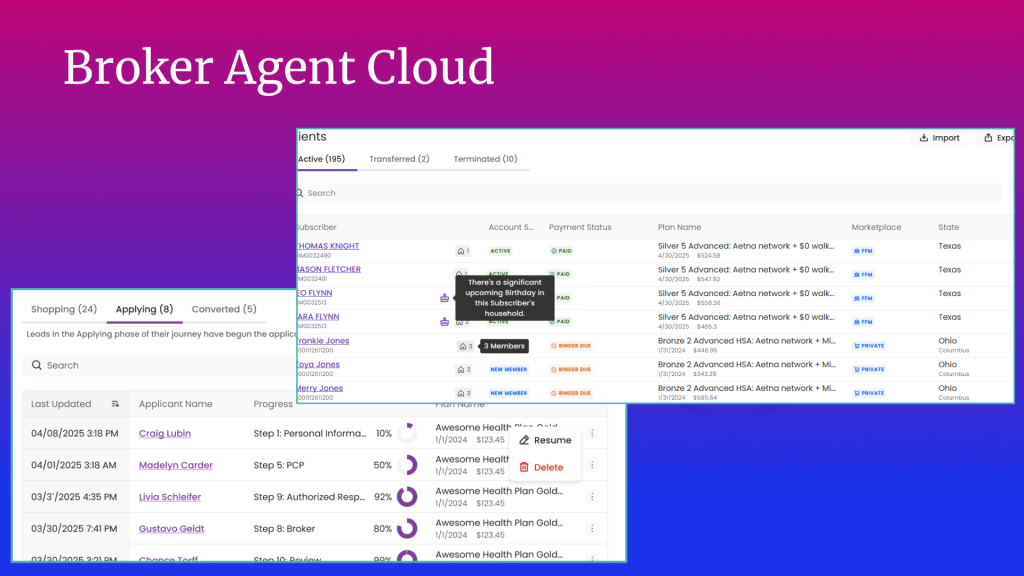
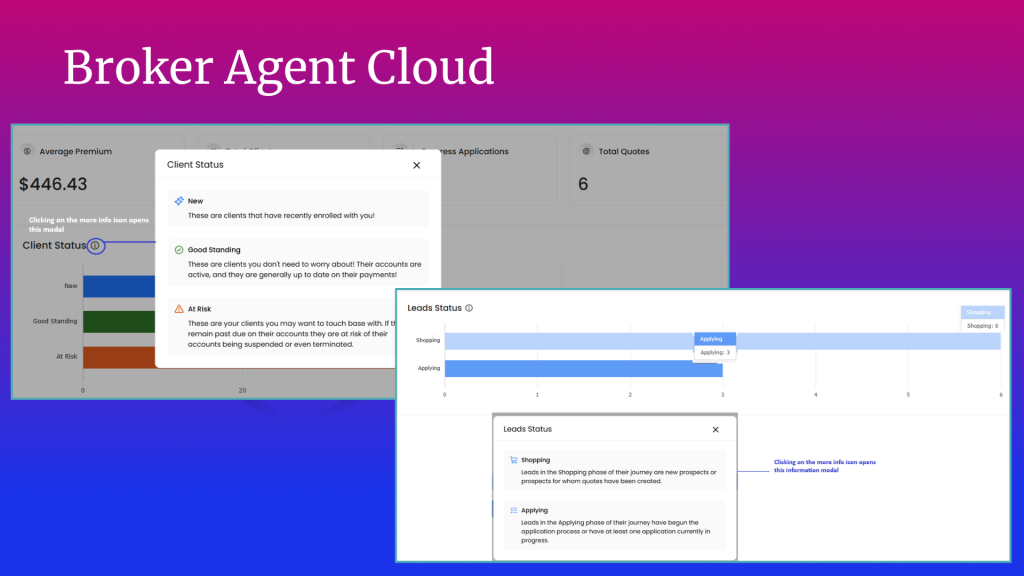
This is where technology can make a real difference. Softheon recently announced Broker Agent Cloud, a new platform designed specifically for benefit advisors. Broker Agent Cloud streamlines quoting, eligibility checks, enrollment, renewals, and payment processing, freeing brokers from manual work so they can focus on guiding members through complex choices.
This aligns with what Lindsey shared during her recent appearance with Spring Street Exchange, where she discussed the need for clear, proactive communication across the broker community. Consistent messaging, early outreach, and plain-language tools will be critical to helping members navigate affordability changes this year.
Communicating Through Uncertainty
Another challenge facing payviders is renewal notices. With no final decision yet on enhanced subsidies, CMS is allowing plans to omit premium and APTC details from 2026 notices. While this prevents members from receiving misleading estimates, it also creates a risk of confusion.
Josh framed the challenge, “Members could be seeing bigger premium increases than they were expecting — and with subsidy levels undecided, plans don’t have the ability to provide complete information. That’s why CMS is giving issuers flexibility this year.”
But as Lindsey noted, payviders cannot afford to let notices stand on their own. “You can’t rely solely on paper notices this year,” she said. “Plans need to leverage brokers, providers, and even community events to get in front of members and make sure they understand what’s changing.”
In practice, this means pairing notices with clear disclaimers directing members to update their information on HealthCare.gov or State-Based Marketplaces (SBMs). Many plans are also supplementing notices with digital campaigns, text reminders, and broker outreach to ensure members know what to expect when their first invoices arrive.
The stakes are high: unclear notices can trigger call center spikes, member abrasion, and even disenrollment. Payviders that take a proactive, multi-channel approach will be better positioned to maintain trust and minimize churn.
Diversifying for the Future
Beyond OE26, diversification remains a strategic imperative. A recent survey found that 51% of healthcare organizations are actively pursuing new revenue opportunities beyond traditional offerings. For payviders, that can mean expanding into ICHRA, introducing supplemental benefits, or even exploring provider-sponsored payments that directly align with mission-driven care.
As Lindsey put it, “It’s not just about revenue. It’s about sustaining the mission and driving access. Any way we can communicate and educate communities about their options is critical to keeping payviders strong.”
Preparing for What’s Next
Heading into OE26, three themes stand out for payviders:
- Stay plugged into regulatory shifts. Court decisions, subsidy extensions, and ICHRA rules will evolve quickly.
- Invest in broker enablement. Confident brokers keep members confident — and enrolled.
- Communicate early and often. Plain-language outreach to members and employers will minimize confusion and build trust.
The affordability threshold changes may be complex, but they also present a chance for payviders to strengthen their role in local communities, expand their offerings, and build resilience for the future.
Watch the full recording of this LinkedIn Live session on YouTube (link) for deeper insights from Marc Bryant, Lindsey Miller, and Josh Schultz. And for more resources on how Softheon partners with payviders to navigate change and expand coverage, visit our Payvider page.


