
August 2025 | By Softheon’s Health Plan Strategy Team
Key takeaways for health plans:
- CMS has issued guidance allowing QHP issuers to omit premium and APTC amounts from renewal notices for the 2026 plan year.
- The enhanced APTCs are set to expire on December 31, 2025, which could lead to increased net premiums for millions of members, and health plans must prepare for potential changes.
- Health plans should prioritize proactive member education and outreach to prepare members for potential changes, including crafting plain-language disclaimers, planning supplemental communications, and leveraging broker and partner channels.
The Centers for Medicare & Medicaid Services (CMS) has issued guidance that gives qualified health plan (QHP) issuers in the individual market some breathing room as they prepare renewal and discontinuation notices for the 2026 benefit year.
This isn’t just another procedural update. The changes come in response to a looming policy shift: the potential expiration of enhanced advance payments of the premium tax credit (eAPTC) at the end of 2025. If Congress doesn’t act to extend them, millions of members could see their subsidies shrink — or disappear — overnight. This would lead to an increase in net premiums that range depending on household characteristics.
With this guidance, CMS aims to prevent confusing information from reaching consumers and reduce the risk of mass uncertainty during the already high-stakes Open Enrollment (OE) period. But for plans, it also means adjusting well-established operational timelines, communication strategies, and customer service playbooks.
What’s Changing in 2026 Notices
Flexibility on Premium & APTC Information
Under federal rules, renewal and product discontinuation notices must include:
- Actual premium for the upcoming year
- APTC amount for the upcoming year
- A comparison to the current year’s amounts
The problem for 2026? eAPTCs — originally created in 2021 under the American Rescue Plan (ARP) and extended by the Inflation Reduction Act (IRA) — are set to expire on December 31, 2025. Using 2025 subsidy amounts in 2026 notices could result in significantly inflated eAPTC figures and underestimated member premiums.
CMS’s fix:
- Issuers may omit premium and APTC amounts in renewal notices for the 2026 plan year, if permitted by their state regulator.
- Issuers can use the 2023 Federal standard template or a forthcoming updated template (once approved federally) that excludes these figures.
This change is designed to avoid member abrasion — that “you told me my premium would be X, but my bill says Y” scenario — and to give plans flexibility during legislative uncertainty.
Enforcement Safe Harbor for Product Discontinuation
CMS will not enforce the requirement for issuers to provide at least 90 days’ notice before discontinuing a product in the individual market, so long as the notice is sent in line with the standard renewal notice timeframe:
- Non-grandfathered, non-transitional plans: before the first day of Open Enrollment
- Grandfathered or transitional plans: at least 60 days before renewal
This accommodation recognizes the tight QHP certification timelines that make 90-day advance notice difficult and aligns discontinuation notices with renewal communications.

State Discretion
While CMS encourages states and State-Based Marketplaces (SBMs) to adopt this flexible approach, they are not required to. Plans must confirm with their primary state regulator whether:
- Omission of premium/APTC figures is permitted
- State-specific notice templates must still be used
Why This Matters Now
The 2026 plan year is shaping up to be one of the most complex renewal seasons since the ACA’s earliest days. The stakes are high, and the uncertainty is real. Unless Congress acts to extend the eAPTCs beyond December 31, 2025, members who have grown accustomed to lower premiums could see their net costs rise sharply.
For some households, particularly those with incomes just over 400% of the Federal Poverty Level, the shift could mean losing subsidy eligibility altogether. Even for those who remain eligible, reduced assistance will limit purchasing power and force difficult trade-offs when comparing plan options for the new year.
For issuers, these changes ripple through every operational and member-facing channel. Higher out-of-pocket costs can trigger a wave of calls from members who are surprised, frustrated, or simply looking for clarity — pushing call centers to their limits during the busiest time of year. The financial shock may also prompt members to shop aggressively, switch to lower-cost plans, or disenroll entirely, adding pressure to retention targets. In this environment, success hinges on more than just timely notices. Plans will need to double down on education, set clear expectations, and provide members with proactive guidance well before the first invoice arrives.
What We Heard from the Softheon User Community
When CMS released the renewal notice guidance, the Softheon User Community — a peer network of operational, compliance, and communications leaders from our health plan partners — came together for a discussion. The goal was straightforward: break down what the guidance means in practice, share initial strategies, and identify potential pitfalls.
Strategic Choices on Notices
A common theme emerged: most plans are leaning toward removing premium and APTC figures entirely from their renewal notices. This approach, permitted under the new CMS flexibility, avoids the risk of displaying outdated or inaccurate subsidy amounts. Instead of potentially misleading members, plans are crafting plain-language disclaimers that direct recipients to HealthCare.gov or their state marketplace to see their actual 2026 rates.
Some are taking the concept a step further, planning follow-up communications once accurate APTC information becomes available later in the season. The logic is simple — if members are going to be surprised, it’s better that it happens with the correct number in front of them.
Outreach & Education Plans
Many participants stressed that the notice is just one piece of the puzzle. Several plans are mobilizing their broker networks as a first line of communication, equipping them with talking points and educational materials so they can guide members through income updates and plan comparisons. Others are launching multi-channel campaigns that go beyond paper notices — using email blasts, text message reminders, portal banners, and even outbound calls to prompt members to review their information and prepare for potential changes. In some cases, marketing teams are designing dedicated campaigns that focus solely on subsidy awareness, aiming to drive engagement before members see their first invoice.
Member Impact Concerns
While the consensus leaned toward omitting cost information, not everyone was convinced it’s a perfect solution. For members accustomed to seeing a dollar amount on their renewal notice, the absence of any cost figure could be just as confusing as an incorrect one. It’s a delicate balance between avoiding misinformation and avoiding an information vacuum.
Another challenge is internal readiness. For many, success means ensuring that call center representatives, broker partners, and other member-facing staff have not only the scripts and FAQs they need but also the deeper understanding to navigate unexpected questions. We can script for these conversations all we want, but there’s always going to be that one question that catches someone off guard.
Insights from Softheon Experts
Our team weighed in with broader context and strategic advice.
Josh Schultz, Head of Government Affairs, noted that this flexibility may signal that CMS is giving time for lawmakers to consider an extension of the enhanced subsidies. “There’s credible talk of health legislation later in the year that could address subsidies,” he explained, “but the timing is uncertain. Plans need to be ready for either outcome.” His point reinforced a reality that weighed heavily over the conversation: operational decisions are being made today under conditions that could change dramatically with a single vote in Congress.
From a client success standpoint, Lindsey Miller, Program Director of Health Plan Solutions, emphasized that renewal season this year cannot be treated as a passive process. “Outreach and education are critical to getting members to engage, update their information, and understand what’s changing,” she said. “The more proactive the plan, the less painful the first invoice shock will be.” Lindsey urged plans to think beyond compliance and view this as an opportunity to build trust — using every available touchpoint to prepare members for the year ahead.
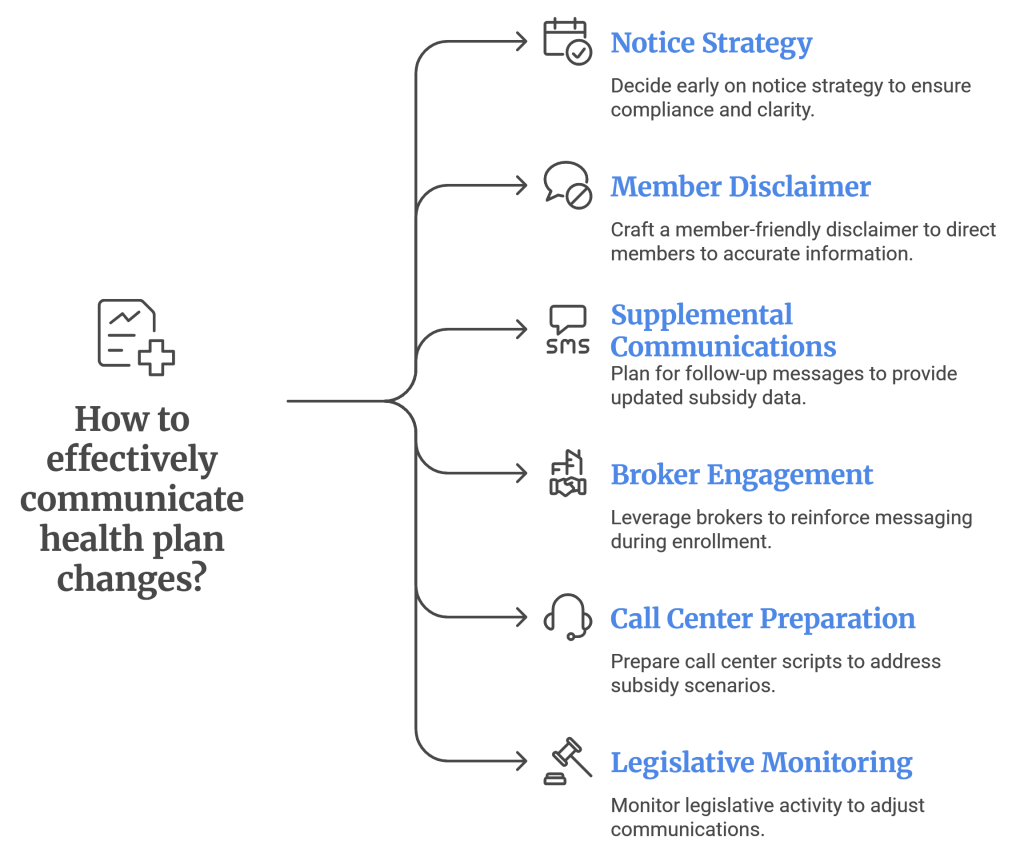
6 Recommendations for Health Plans
- Decide Early on Your Notice Strategy — Confirm with your state whether omitting premium/APTC amounts is permissible, and lock in your template choice.
- Craft a Member-Friendly Disclaimer — Direct members to HealthCare.gov or the state exchange for accurate, updated figures. Keep the language plain and actionable.
- Plan for Supplemental Communications — If possible, send follow-up notices or digital messages once accurate subsidy data becomes available.
- Leverage Broker and Partner Channels — Train brokers and agents to reinforce the message during enrollment conversations.
- Prepare Your Call Center — Develop scripts and FAQs that address both scenarios — with and without extended subsidies.
- Monitor Legislative Activity — Assign internal resources or rely on vendor partners to track Congressional action on the eAPTCs and adjust communications accordingly.
Looking Ahead
CMS’s guidance is a rare mix of operational flexibility and regulatory clarity in a year clouded by uncertainty. It buys issuers time — but not a pass on member communication. Whether enhanced subsidies are extended, reduced, or allowed to expire, the real test will be how well plans prepare their staff, partners, and members for the transition.
At Softheon, we’ll continue to share updates from D.C., provide template and scripting support, and facilitate peer-to-peer discussions in our User Community. Together, we can navigate 2026’s challenges with fewer surprises and a smoother member experience.
If you have questions about how this changing notice guidance will impact your member communication for OE26, reach out to our team here.


